Knee
- Patellar Tendon Injuries
- Patellar Tendon Treatment Options
- Patient Resources
Patellar Tendon Injuries
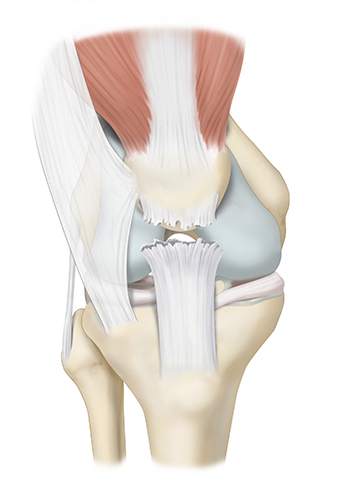
The knee joint is supported by several important tendons, which play a crucial role in stabilizing and facilitating the movement of the knee. The patellar tendon connects the patella (kneecap) to the tibia (shinbone). It plays a central role in straightening the knee and is essential for activities like standing, walking, and running.
The patellar tendon is part of a larger biomechanical structure called the knee extensor mechanism. The knee extensor mechanism is comprised of the patellar tendon, quadriceps tendon, quadriceps muscle group, and the patella. Together, these anatomical structures work to facilitate extension (straightening) of the knee and stability to the knee joint.
What is a patellar tendon rupture?
A patellar tendon rupture is characterized by a complete or partial full thickness tear of the patellar tendon. The patellar tendon is a strong, flat band of tissue connecting the patella to the tibial tuberosity, which is a bony prominence of the tibia. The patellar tendon transmits forces generated by the quadriceps muscles to the tibia, which allows for knee extension. Thus, in cases of patellar tendon ruptures, patients’ ability to extend the leg, walk, run, or jump will likely be compromised.
What causes a patellar tendon rupture?
Patellar tendon ruptures are typically caused by a sudden, powerful contraction of the quadriceps muscle in your thigh. This can happen from a fall or during activities like jumping, landing, or sudden stops. Chronic overuse and degenerative changes can also contribute to patellar tendon injury, especially in older individuals.
What are the symptoms of a patellar tendon rupture?
- Severe pain in the front of the knee, typically below or around the kneecap.
- Swelling of the knee
- Inability to straighten your knee/perform a straight leg raise.
- Inability to bear weight on the leg.
- A noticeable gap or divot just below the kneecap
- Possible migration of the patella upwards.
How is a patellar tendon rupture diagnosed?
Diagnosis of Patellar Tendon Injuries
Accurate diagnosis of a patellar tendon injury typically requires a combination of a comprehensive physical examination, x-rays, and an MRI. Dr. Bryan Penalosa and his team will begin with a detailed physical exam, which includes palpating the knee to detect any tendon gap or divot, assessing your ability to perform a straight leg raise, and evaluating overall range of motion.
X-rays are often obtained to rule out fractures and to assess the position of the patella, including identifying patella alta (upward migration of the kneecap). An MRI provides the most detailed assessment, allowing Dr. Bryan Penalosa to determine the severity of the tendon injury and to identify any additional ligament, meniscal, or cartilage damage that may be present.
Patellar Tendon Treatment Options
Can a patellar tendon rupture be treated without surgery?
In some cases, a partial rupture of the patellar tendon may be treated non-surgically with rest, immobilization using a hinged knee brace locked straight, and physical therapy. A platelet rich plasma (PRP) injection directly to the affected tendon can also help relieve knee pain and promote healing of the partial thickness tearing of the tendon. Moreover, extracorporeal shock wave treatments have also been shown to produce good outcomes.
However, it is important to note that complete patellar tendon ruptures often require surgical repair to regain full knee function. Additionally, even in cases of a partial patellar tendon rupture, if you cannot perform a straight leg raise, surgical intervention will likely be recommended.
What are the surgical options for a patellar tendon rupture?
Surgical options for patellar tendon ruptures typically involve reattaching the torn patellar tendon to the patella using sutures or non-metal anchors. The choice of surgical technique depends on the extent of the injury and the characteristics of the tissue. Bone tunnels [33-3] and anchors [33-2] can be used and have demonstrated excellent long-term outcomes.
In cases of more severe injury or chronic injury to the patellar tendon, Dr. Bryan Penalosa may recommend reconstructing the tendon using either an Achilles tendon allograft (donor tissue) or a biologics patch known as Regeneten. Regeneten is a collagen-based implant that supports the body’s natural healing response to facilitate new tendon-like growth and reduce strain at the site of the patellar tendon tear. Regeneten is composed of Type 1 collagen and has been shown for up to 5 years to increase and maintain the repaired patellar tendon thickness.
How long is the recovery after a patellar tendon repair/reconstruction?
Initially following the surgical repair of the patellar tendon, you will be allowed to bear full weight on the operative leg using crutches as tolerated by pain. You will be required to wear a hinged knee brace for 6 weeks following surgery. Initially, this brace will be locked straight. Physical therapy will begin immediately following surgery, and you will be allowed to gradually progress the range of motion of the operative knee over a period of 6 weeks per Dr. Bryan Penalosa’s patellar tendon repair/reconstruction post-operative protocol. Physical therapy is a crucial part of the recovery process to regain strength and mobility. Full recovery can take six months to a year.
What are the long-term effects of an untreated patellar tendon rupture?
An untreated patellar tendon rupture can lead to chronic knee pain, weakness, and a significant loss of knee function. It can also increase the risk of developing osteoarthritis in the affected knee over time. Therefore, prompt treatment is crucial to prevent long-term complications.
Patient Resources
Orthopedic surgeon Dr. Bryan Penalosa and his team are dedicated to providing an industry-leading patient experience—one that is smooth, efficient, and convenient. Our team has compiled a comprehensive set of orthopedic patient resources to assist you with insurance information, patient forms, and much more.
Explore the patient resources below to learn more.
- Preparing for Surgery
- Traveling for Surgery
- Pre-Operative Clearance
- Peri-Operative Nutrition
- Post-Operative Instructions
- Post-Operative Physical Therapy
- Post-Operative Medications
- Durable Medical Equipment
- Billing & Insurance
- Patient Portal
- Medical Records
- Patient IQ
- Clinical Case and Imaging Review
- Ongoing Clinical Trials
- Sports Performance Center
