Knee
- Patellar Instability
- Patellar Instability Treatment Options
- Effects of Untreated Patellar Instability
- Patient Resources
Patellar Instability
What is patellar instability?
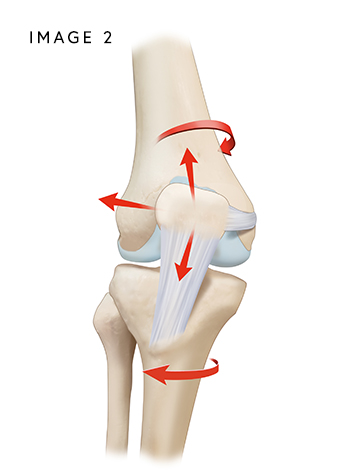
The patella (kneecap) fits into a groove at the end of the femur (thigh bone) and glides up and down as the knee bends and straightens. Several ligaments and soft-tissue structures help keep the patella properly aligned and tracking within this groove.
The primary stabilizer of the kneecap is the medial patellofemoral ligament (MPFL). The MPFL connects the inner side of the patella to the medial femoral condyle, a bony prominence on the inner aspect of the femur. Its main function is to keep the patella from drifting outward and to maintain its position in the trochlear groove.
The lateral patellofemoral ligament (LPFL) attaches to the outer edge of the patella and anchors to the lateral femoral condyle, helping prevent excessive inward shift of the kneecap.
In addition, the quadriceps tendon connects the quadriceps muscle to the patella, and the patellar tendon connects the patella to the tibia (shinbone), forming the extensor mechanism responsible for straightening the knee.
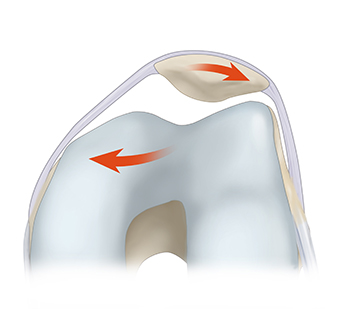
When the patella becomes unstable, it can dislocate or slip out of the groove. This leads to pain, swelling, stiffness, and a feeling of the knee “giving way.” When the kneecap slips out of the trochlea, the condition is known as patellofemoral instability (PFI).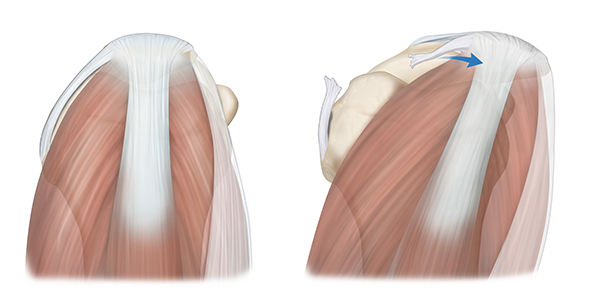
What causes patellar instability?
Acute kneecap dislocation and patellar instability is frequently the result of a sports injury, a fall, or a direct impact to the joint that forces the patella out of its normal “track.” Frequently, this is the result of an underlying preexisting condition such as an abnormally high kneecap (patella alta), a shallow groove (trochlear dyplasia), or misalignment of the kneecap and tibia (increased q angle, rotational deformities, etc.), among other abnormalities.
How common are patellar dislocations?
Women and girls have naturally loose ligaments, which predisposes them to lateral patellar dislocation, a common injury in young, active girls and women. Lateral patellar dislocations are the most common knee dislocation injury among young adults, leading to an injury to the MPFL.
Am I at risk for a recurrent patellar dislocation?
The risk of a second dislocation is high after an initial injury, dislocation, or subluxation (partial dislocation) of the patella. Approximately, 15 to 44% of patients who suffer a traumatic dislocation will have recurrent dislocations. Two or more dislocations increase the recurrence rate to over 50%.
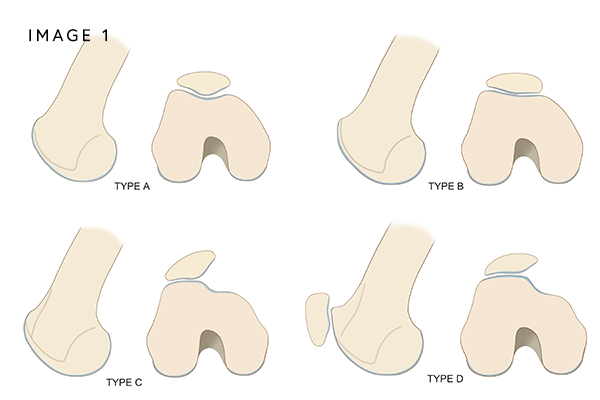
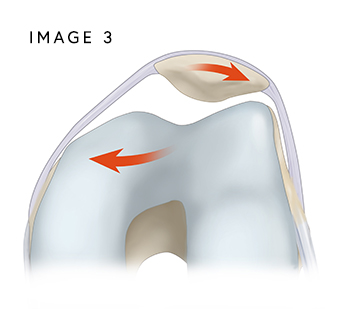
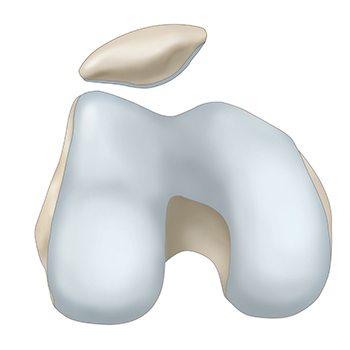
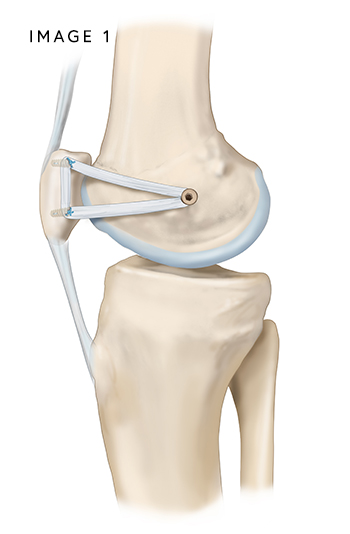
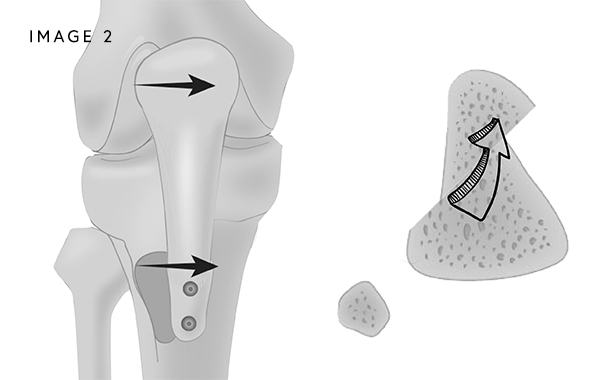
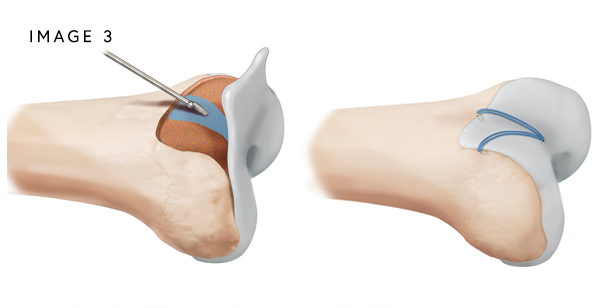
Repeated dislocations are not the result of trauma. Instead, they are caused by a shallow groove (trochlear dysplasia) (Image 1) a kneecap that sits too high (patella alta) (Image 2), bone abnormalities (Image 3), lax muscles (Image 4), ligament injuries including a torn or stretched MPFL, weak quadriceps muscles, and tight hip flexors. Additional risk factors for recurrent instability include young age and sports-related injuries.

What are the symptoms of patellar instability?
Chronic patellar instability is very painful and can significantly limit participation in physical activities due to fear of recurrent dislocations. People who have kneecap instability typically have symptoms that include:
- Swelling and bruising
- Pain while sitting and standing up.
- Pain in the front of the knee
- Joint stiffness
- Knee buckling and catching.
- A creaking sound with knee motion
- Difficulty walking
How is a patellar instability diagnosed?
A combination of a comprehensive history of prior patellar instability episodes, physical examination, X-rays, and an MRI or CT scan is used to diagnose patellar instability. Dr. Bryan Penalosa and his team will perform a physical exam that includes observing how the kneecap moves throughout its range of motion.
An X-ray will be obtained to assess for bony abnormalities that may predispose you to patellar instability, such as patella alta (a high-riding kneecap). An MRI will be ordered to evaluate soft tissue structures, including the MPFL and LPFL, to determine if either ligament is torn. The MRI will also help identify any loose bodies within the joint or bone bruising caused by contact between the patellar facet (edge of the kneecap) and the femoral condyle during a dislocation or instability event.
In some cases, a CT scan may be used to determine whether the bones are properly aligned or if rotational or structural abnormalities are contributing to patellar instability.
Patellar Instability Treatment Options
Can patellar instability be treated without surgery?
In acute cases of instability, including the first injury to the MPFL or LPFL, conservative treatment may be recommended. This includes physical therapy to restore strength and mobility, as well as the temporary use of a knee brace. Conservative treatment with a period of immobilization followed by physical therapy can be beneficial in some patients depending on their underlying predisposing factors. However, despite conservative treatment, recurrent dislocations can still occur. Even without recurrent dislocations, persistent problems, disability, and arthritis can be present. Thus, MPFL or LPFL reconstruction may be offered early to prevent these consequences when a patient has recurrent dislocations.
What are the surgical options for patellar instability?
Treatment for chronic knee instability is focused on correcting the underlying cause. The goal is to restore stability. Surgical treatment options are based on the cause of the chronic instability.
- When instability is caused by complex issues like a ligament tear or laxity, surgical reconstruction of the MPFL or LPFL will be recommended to enable the kneecap to track properly and remain in its groove. (Image 1)
- When there is a misalignment of the bones, a surgical procedure called an osteotomy may be recommended to realign the bones and prevent future dislocations. (Image 2)
- When there is a big jump of the knee cap a surgery called trochleoplasty may need to be performed (Image 3)
- When there is cartilage damage, surgery to reposition the kneecap and give it more space to move with respect to the femur can improve the pain.
- If needed, knee arthroscopy and cartilage restoration procedures can help by stabilizing fragments of cartilage that might be loose.
How long is the recovery after MPFL/LPFL Reconstruction?
Post-Operative Care After Patellar Instability Surgery
Immediately after patellar instability surgery, you will be allowed to bear full weight on the operative leg while using crutches, as tolerated by pain. A hinged knee brace must be worn for the first 6 weeks after surgery. In the early phase, this brace will be locked in full extension (straight).
Physical therapy begins right away after the procedure. Under Dr. Chahla’s MPFL/LPFL reconstruction post-operative protocol, your range of motion will gradually increase over the first 6 weeks. Physical therapy plays an essential role in restoring strength, stability, and mobility.
A complete recovery typically takes 4–7 months, depending on individual progress and adherence to rehabilitation guidelines.
Effects of Untreated Patellar Instability
What are the long-term effects of untreated patellar instability?
Long-term complications of patellar instability, especially if patellar instability is not properly managed or if patellar instability episodes occur repeatedly include:
Recurrent Dislocations:
Once a person has experienced a patellar dislocation, they may be at a higher risk of having more dislocations in the future. Repeated dislocations can cause further damage to the knee joint.
Patellofemoral Instability:
Patellar dislocations can result in chronic patellofemoral instability, where the patella doesn’t track properly within the femoral groove, leading to ongoing pain and functional limitations.
Cartilage Damage:
During a patellar dislocation, the patella may scrape against the femur or other structures, potentially causing cartilage damage. Over time, this can lead to osteoarthritis in the knee joint.
Ligament or Tendon Injuries:
The initial dislocation may also damage ligaments, tendons, or other soft tissues in the knee, which can affect joint stability and function.
Muscle Weakness:
Following a patellar dislocation and associated injuries, there may be muscle weakness in the quadriceps and other leg muscles, which can further contribute to instability and functional limitations.
Chronic Pain:
Persistent pain can result from patellar dislocations, especially if there is ongoing instability or damage to the joint structures.
Reduced Range of Motion:
Some individuals may experience a limited range of motion in the knee joint due to scarring, inflammation, or damage caused by dislocations.
Patient Resources
Orthopedic surgeon Dr. Bryan Penalosa and his team are dedicated to providing an industry-leading patient experience—one that is smooth, efficient, and convenient. Our team has compiled a comprehensive set of orthopedic patient resources to assist you with insurance information, patient forms, and much more.
Explore the patient resources below to learn more.
- Preparing for Surgery
- Traveling for Surgery
- Pre-Operative Clearance
- Peri-Operative Nutrition
- Post-Operative Instructions
- Post-Operative Physical Therapy
- Post-Operative Medications
- Durable Medical Equipment
- Billing & Insurance
- Patient Portal
- Medical Records
- Patient IQ
- Clinical Case and Imaging Review
- Ongoing Clinical Trials
- Sports Performance Center
