Knee
- MCL Injuries
- MCL Injuries Non-Surgical Treatment
- MCL Injuries Surgical Treatment
- Recovering from MCL Surgery
- Patient Resources
MCL Injuries
What is the medial collateral ligament (MCL)?
The MCL is a structure that stabilizes the medial side (inside) of the knee, connecting the thigh bone (femur) to the shinbone (tibia). The MCL prevents forces applied to the lateral (outside) side of the knee from gapping open the inside of the knee (valgus stress).
The posteromedial corner of the knee is comprised of the MCL and the posterior oblique ligament (POL). Both structures control the stability and valgus stress of the knee.
The MCL and the POL prevent the knee from gapping open when the tibia internally rotates. The MCL functions when the knee is slightly flexed (20 to 30 degrees of flexion) whereas the POL (more to the back of the knee) functions close to extension (0 degrees of flexion). The different roles of each of these ligaments help to ensure the stability of the knee to valgus stress throughout a full range of motion.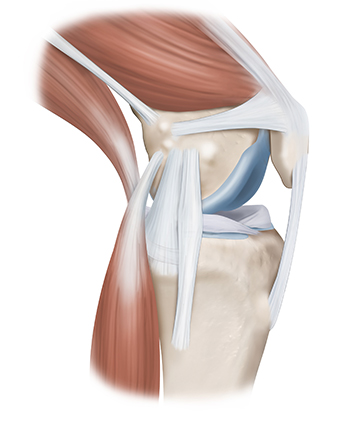
What causes MCL injuries?
MCL injuries can result from twisting injuries, causing the knee to buckle and gap open on the inside of the knee. MCL injuries can also result from contact injuries, like a blow to the outside of the knee, causing valgus gapping. MCL injuries are very common with almost 750,000 injuries occurring every year in the United States. Overall, MCL tears are two to three times more common than ACL tears.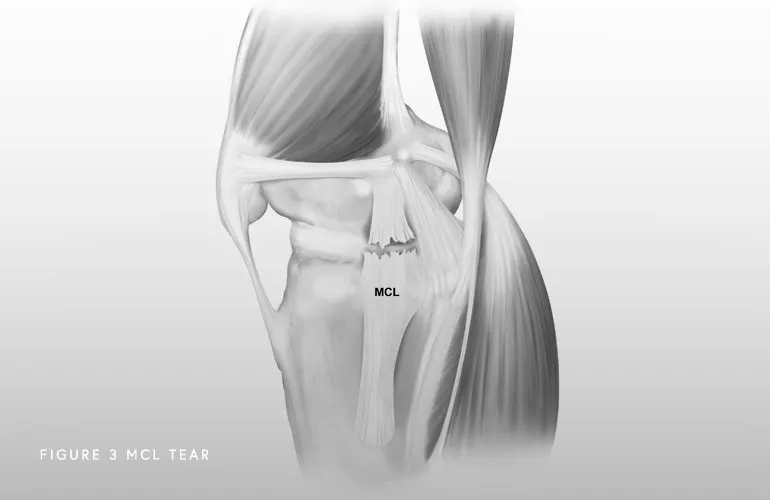
What are the symptoms of an MCL injury?
Symptoms depend on the severity of the injury. A mild injury (grade I or II) might present with pain over the ligament attachments. In more severe cases, patients feel that their knee can give out or buckle. Below are some of the most common symptoms of an MCL injury:
- Pain: Pain on the inner side of the knee is a common symptom of a torn MCL. The pain may range from mild to severe, depending on the extent of the injury.
- Swelling
- Stiffness: The knee may become stiff, making it difficult to fully bend or straighten the leg.
- Instability: An individual with a torn MCL may feel that the knee is unstable, as if it’s “giving way” or unable to support their weight properly.
- Bruising: Bruising can develop around the site of the MCL tear, and the discoloration is often seen on the inner side of the knee.
- Difficulty Walking: Walking may be uncomfortable or painful, particularly if the MCL tear is severe.
- Popping or Clicking Sensation: Some people report a popping or clicking sensation when the injury occurs, which may be followed by pain and swelling.
How is an MCL injury diagnosed?
A combination of a comprehensive physical examination, special x-rays, and an MRI are usually very accurate. Dr. Bryan Penalosa and his team will perform a physical exam that will include testing your knee in an extended (straight) and flexed position to determine the location and severity of the injury. A special x-ray, called a valgus stress x-ray, will likely be obtained. This special x-ray allows Dr. Bryan Penalosa to objectively quantify and diagnose (based on validated systems) a posteromedial corner injury with millimeter accuracy. An MRI will allow Dr. Bryan Penalosa to further evaluate the extent of the MCL injury as well as to evaluate the knee for any concomitant ligament, meniscal, or cartilage injuries.
MCL Injuries Non-Surgical Treatment
Can an MCL injury be treated without surgery?
Isolated MCL tears commonly heal on their own because they have a very robust supply of blood flow and nutrients. Additionally, this ligament is outside the knee joint capsule (the lining of the joint). Proteins within the joint fluid inhibit healing, so therefore, being outside the joint is beneficial for healing. Moreover, on the inside, or medial aspect, of the knee, the convex (rounded) end of the femur articulates with a concave (bowl-shaped) tibia, which allows for a more stable joint.
Non-operative treatment of MCL injuries involves a change in activities to avoid movements that cause knee pain, instability, and excessive valgus stress to the knee. Additional conservative treatment options include over-the-counter anti-inflammatory medications to reduce pain and inflammation, use of a hinged knee brace, and physical therapy. Typically, symptoms will resolve within 2-4 months of conservative, non-surgical treatment. If your knee pain is resolved with non-operative treatment and you can return to your desired level of activity, then no MCL surgery is needed.
However, there are two situations in which the MCL will not heal. First, if the knee gaps open on the inside when the knee is fully extended (valgus gapping in extension), the likelihood of the MCL healing without surgery is very low. The reason for this is that it is likely that both the MCL and POL are injured. The second type of injury requiring surgery is a tear of the MCL at the tibial attachment that retracts toward the knee. This is called a meniscotibial MCL tear. These types of tears also usually don’t heal on their own. This is because the torn and retracted MCL becomes trapped above the hamstring tendons, and it cannot heal back down to the tibia. In both types of injuries, the knee will feel very unstable to inward pressure (valgus force) when assessed by a physician.
MCL Injuries Surgical Treatment
What are the surgical options for an MCL injury?
When there is a complete tear of the MCL (Grade 3) or when all the structures of the posteromedial corner of the knee are injured, surgery should be performed within two weeks after injury and once range of motion has been recovered. This is the best time to repair the structures because significant scarring and tissue weakening has not yet occurred. The position and alignment of the knee can also be anatomically restored during that time frame, rather than delaying and allowing the knee to heal in an abnormal position. Recent reconstruction techniques have allowed many patients to get back to high-level activities.
Restoring the native anatomy of the MCL and posteromedial corner can allow for early postoperative range of motion and produce better outcomes. There are multiple techniques described to do this, including augmentation procedures (meaning that a graft is utilized to supplement your own tissue) or full reconstruction. Full reconstruction includes use of a graft to reconstruct the MCL or all the components of the posteromedial corner (MCL and POL), depending on the degree of the injury.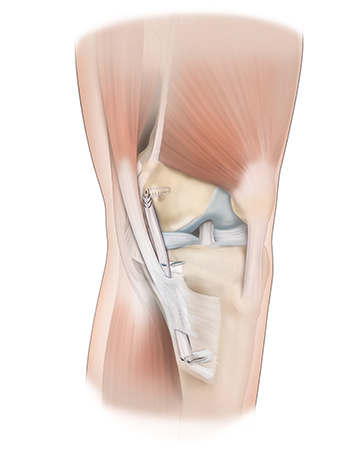
Recovering from MCL Surgery
How long is the recovery after MCL surgery?
Depending on the severity of the MCL injury and the associated ligaments injured, recovery following MCL surgery can take between 6 and 12 months. Physical therapy starts on postoperative day 1 or 2 to work on range of motion. Patients should not bear weight (or very little weight bearing) for the first six weeks after surgery. Driving on the operative knee is usually allowed at about seven to eight weeks postoperatively. Endurance and strengthening can be started in the second phase of the rehabilitation. Agility exercises start at 4 months post-op, along with the running progression if previous stages have been successfully achieved. Return to sport following an MCL surgery is typically at 9 months post-op.
Patient Resources
Orthopedic surgeon Dr. Bryan Penalosa and his team are dedicated to providing an industry-leading patient experience—one that is smooth, efficient, and convenient. Our team has compiled a comprehensive set of orthopedic patient resources to assist you with insurance information, patient forms, and much more.
Explore the patient resources below to learn more.
- Preparing for Surgery
- Traveling for Surgery
- Pre-Operative Clearance
- Peri-Operative Nutrition
- Post-Operative Instructions
- Post-Operative Physical Therapy
- Post-Operative Medications
- Durable Medical Equipment
- Billing & Insurance
- Patient Portal
- Medical Records
- Patient IQ
- Clinical Case and Imaging Review
- Ongoing Clinical Trials
- Sports Performance Center
